The Role of Advanced Illness Management in Compassionate Care
January 01, 2025
Advanced illness management plays a critical role in ensuring that patients facing severe health challenges receive the compassionate care they deserve. By focusing on the needs of both the patient and their families, this approach strives to improve quality of life, alleviate symptoms, and provide support through challenging times. In this blog, we explore the essential components of advanced illness management and how it contributes to a compassionate care model.
Understanding Advanced Illness Management
Advanced illness management is a specialized approach to care that aims to address the complex needs of patients with serious health conditions. It encompasses a range of services designed to improve quality of life and manage symptoms effectively.
One of the main goals of advanced illness management is to create a comprehensive care plan that considers not only the medical needs but also the personal wishes and values of patients. This approach involves detailed discussions and planning sessions with patients and their families to ensure that every aspect of care is aligned with the patient’s goals. This personalized care planning becomes particularly important in managing complex health conditions and steering clear of unnecessary medical interventions, ultimately preserving the patient’s independence and quality of life. By doing so, it allows patients and families to focus more on meaningful interactions rather than medical logistics.
The principle of advanced illness management revolves around empathy and respect. It aims to deliver care that listens to the patient’s voice, ensuring that their needs and preferences are prioritized in decision-making. This involves not only healthcare providers but also involves equipping families with resources and guidance on care options, facilitating a supportive and informed environment. It’s about making sure that as patients face the complexities of serious illness, they’re surrounded by care that truly sees them as individuals with unique stories and needs. This concerted effort significantly enhances the ability to navigate the healthcare landscape with dignity and comfort.
Key Components of Compassionate Care
Compassionate care involves recognizing the physical, emotional, and psychological needs of patients. It includes comprehensive care planning, effective communication, and respectful treatment to ensure that patients feel valued and understood.
Central to compassionate care is the art of listening and engaging with patients and their families in a way that fosters trust and understanding. This involves acknowledging the emotional weight of a diagnosis and providing a safe space for patients and their families to express concerns and ask questions. When healthcare providers cultivate such an environment, it improves not only the treatment experience but also patient satisfaction. Open and empathetic communication serves as the cornerstone of this model, helping to build a relationship that is transparent and collaborative, ultimately leading to better health outcomes.
Integrating spirituality and holistic segments into the care model further exemplifies compassionate care. Many patients find strength in spiritual and psychological counseling, which can greatly assist in dealing with the stress and challenges of illness. By offering these services alongside the physical treatment of symptoms, healthcare teams can enhance the overall healing experience. Moreover, involving spiritual advisors and mental health professionals in the care delivery process helps address varied patient needs, whether through one-on-one conversations, support groups, or tailored therapy sessions.
The Importance of Patient-Centered Care
Patient-centered care lies at the heart of advanced illness management, focusing on individual preferences and values. By tailoring care plans to each patient’s unique needs, healthcare providers can offer more effective and compassionate support.
Tailoring care to individual needs requires healthcare providers to deeply understand the patient’s lifestyle, support system, and preferences. This involves detailed assessments and open dialogues that lead to a personalized care plan suiting their unique circumstances and goals. Advanced care planning is more than administrating treatments; it’s about partnership with the patient at every stage of care. Personalized plans can include various interventions, from medical treatments to alternative therapies, which align with the patient’s philosophies and expected quality of life enhancements. Such customization ensures that patients remain at the center of their own care decisions.
The significance of patient-centered care is further emphasized by its ability to empower patients. When healthcare providers respect and incorporate patients’ inputs, it fosters a greater sense of autonomy and confidence among patients. This empowerment transcends mere symptom management—patients who are involved in their care usually experience better engagement, are motivated to follow through with treatment regimens, and often have better recovery rates. This approach establishes a sense of agency, making patients active participants in their healthcare journey and not just passive recipients of care.
The Role of Multidisciplinary Teams
Successful advanced illness management involves collaboration among various healthcare professionals. Multidisciplinary teams work together to provide comprehensive, coordinated care that addresses both medical and supportive needs of patients and their families.
These teams are often composed of a diverse group of specialists—doctors, nurses, therapists, social workers, and spiritual advisors—each bringing expertise that is essential to managing different facets of a patient’s care. By integrating these roles, the team can deliver a robust, all-encompassing care plan catering not just to immediate health needs but also to emotional, social, and psychological aspects. This collaborative approach ensures that all dimensions of patient care are explored and managed in harmony, preventing gaps and overlaps that could undermine care quality.
The advantage of a multidisciplinary team lies in its strength to address sudden changes in patient conditions efficiently. Real-time communication channels allow for swift adjustments to be made in the care plan, responding adaptively to new symptoms or complications. This continuous monitoring and iterative updating of patient care plans make the team dynamic and responsive. As a result, patients benefit from a seamless care experience, whether that involves a tweaking of medication dosages, introducing new therapies, or facilitating hospital-home transitions.
Enhancing Quality of Life Through Symptom Management
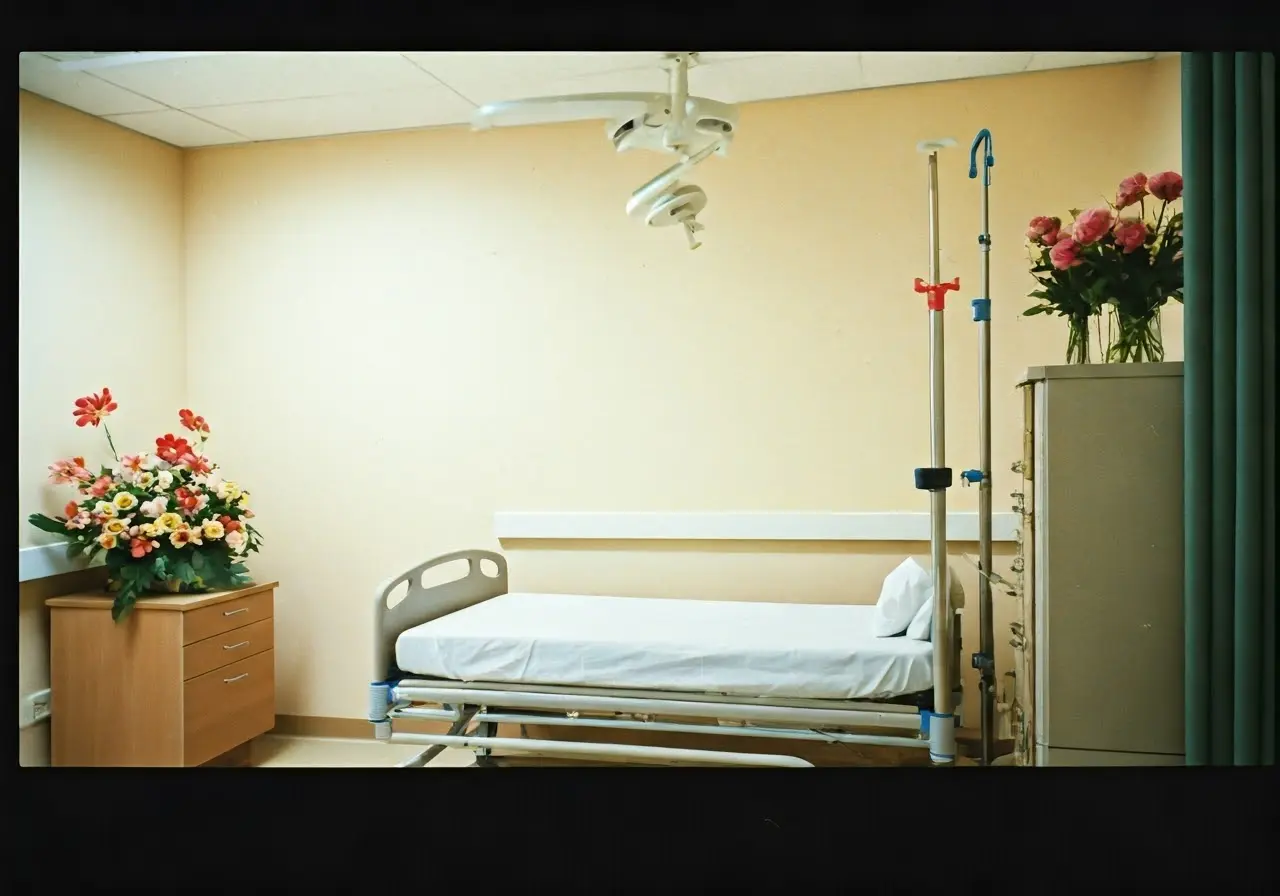
Effective symptom management is crucial in advanced illness care. By alleviating pain and other distressing symptoms, healthcare providers can significantly enhance the quality of life for patients, allowing them to focus on meaningful activities.
Pain and symptom management are pivotal in maintaining patient comfort during illness management. Through the use of targeted pain relief methods, ranging from medications like opioids to non-pharmacologic interventions such as acupuncture and massage, patients can experience considerable relief from persistent symptoms. Not only does this allow them to participate more actively in daily routines, it also contributes to emotional well-being. Comprehensive symptom management strategies are tailored individually, often building on patients’ treatment history, tolerances, and preferences to find the most effective approach.
Beyond managing immediate pain, it is important to address other symptoms that could affect a patient’s daily life, such as nausea, fatigue, and shortness of breath. An integrated approach facilitates attention to these symptoms, with nutritionists, physiotherapists, and other specialists joining forces to provide holistic care. This collaboration often results in specialized interventions—be it dietary alterations or breathing exercises—that proactively target these discomforts, offering substantial improvements in day-to-day functioning and overall quality of life.
Providing Emotional and Psychological Support
Emotional and psychological support is a vital aspect of compassionate care. By offering counseling, support groups, and open communication, healthcare providers can help patients and families navigate the emotional challenges associated with advanced illness.
Navigating advanced illness often brings emotional turmoil, not just for patients but also for their families. Providing a strong support network helps mitigate these challenges. Healthcare providers focus on creating an environment where patients feel safe to express their fears, hopes, and even uncertainties. Whether through one-on-one counseling sessions, family therapy, or peer support groups, emotional care seeks to stabilize and uplift patients, reducing feelings of isolation and trepidation. This psychological support aids in better managing the overall stress of the illness and contributes to a more profound sense of peace.
Incorporating psychological support into patient care plans involves a team of mental health professionals working closely with individuals to develop coping strategies that align with their lives and values. Introducing techniques like mindfulness, cognitive behavioral therapy, or spiritual guidance can significantly influence emotional health, providing much-needed relief and resilience. By addressing the mental aspects of illness head-on, caregivers help transform daunting health challenges into manageable experiences, enabling patients to maintain autonomy and dignity during their care journey.
Embracing Advanced Illness Management for Compassionate Care
Advanced illness management is fundamental to providing compassionate care for patients with serious health conditions. By prioritizing patient comfort, coordinating comprehensive care, and offering emotional support, this approach fosters an environment of understanding and empathy. As we move forward, integrating advanced illness management into standard care practices will be crucial in ensuring that every patient receives the dignity and care they deserve. To learn more about how we can support you and your loved ones, visit our homepage.
Filed under:
Articles and Resource Topics

A Registered Nurse is available to answer your questions about hospice and palliative care services:
- Discuss your unique situation to determine how Inspire services can be tailored to care for you and your family
- Discuss insurance, Medicare and answer other concerns about eligibility, benefits, and other care options
- Answer any questions you have about comfort care